Funded Research
Adult Projects
Pediatric Projects
Total Projects
Research News

Local Support Creating Global Impact

Pedal the Cause Pushes Pediatric Cancer Research Forward

Eight new cancer research projects and one clinical trial funded by Pedal the Cause
The Multiplier Effect
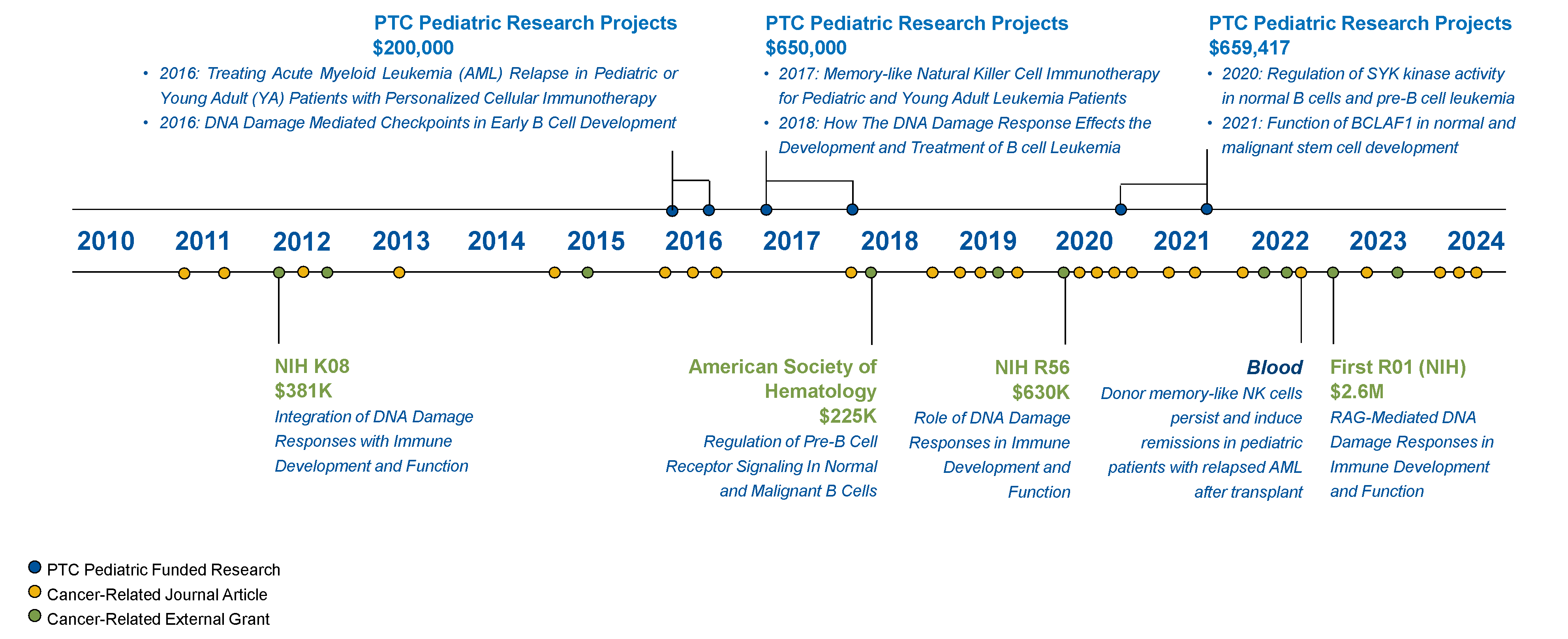
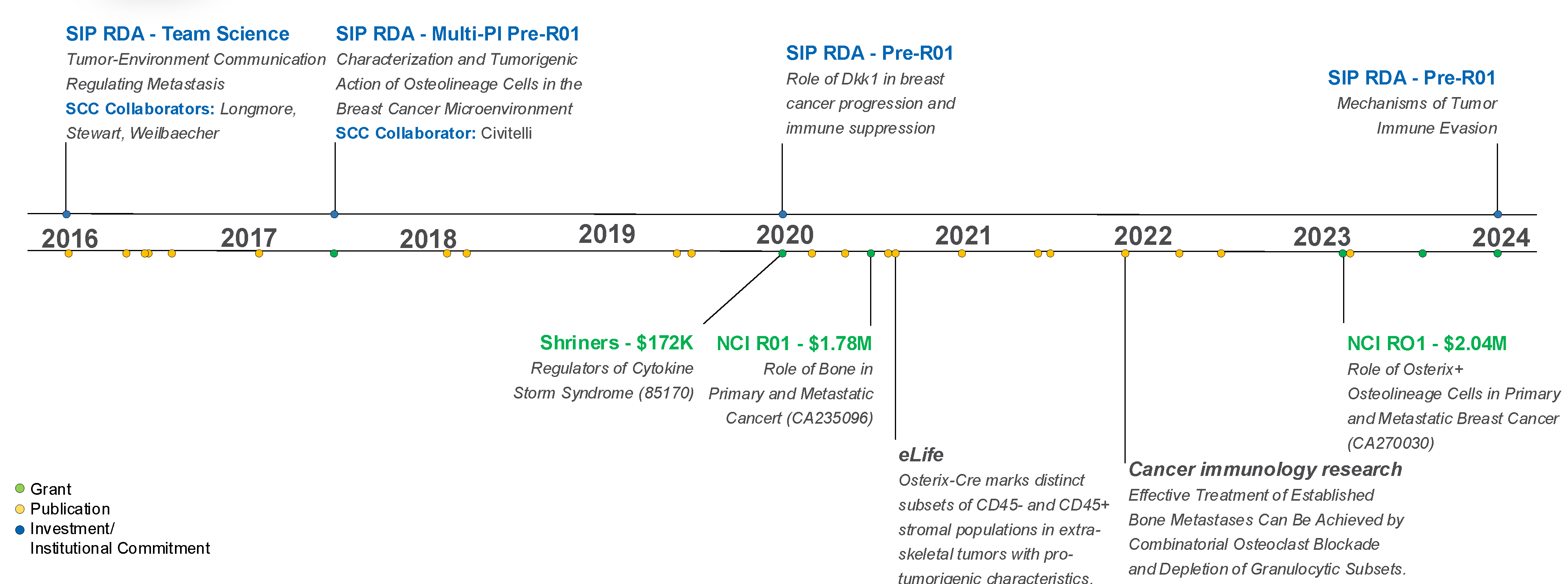
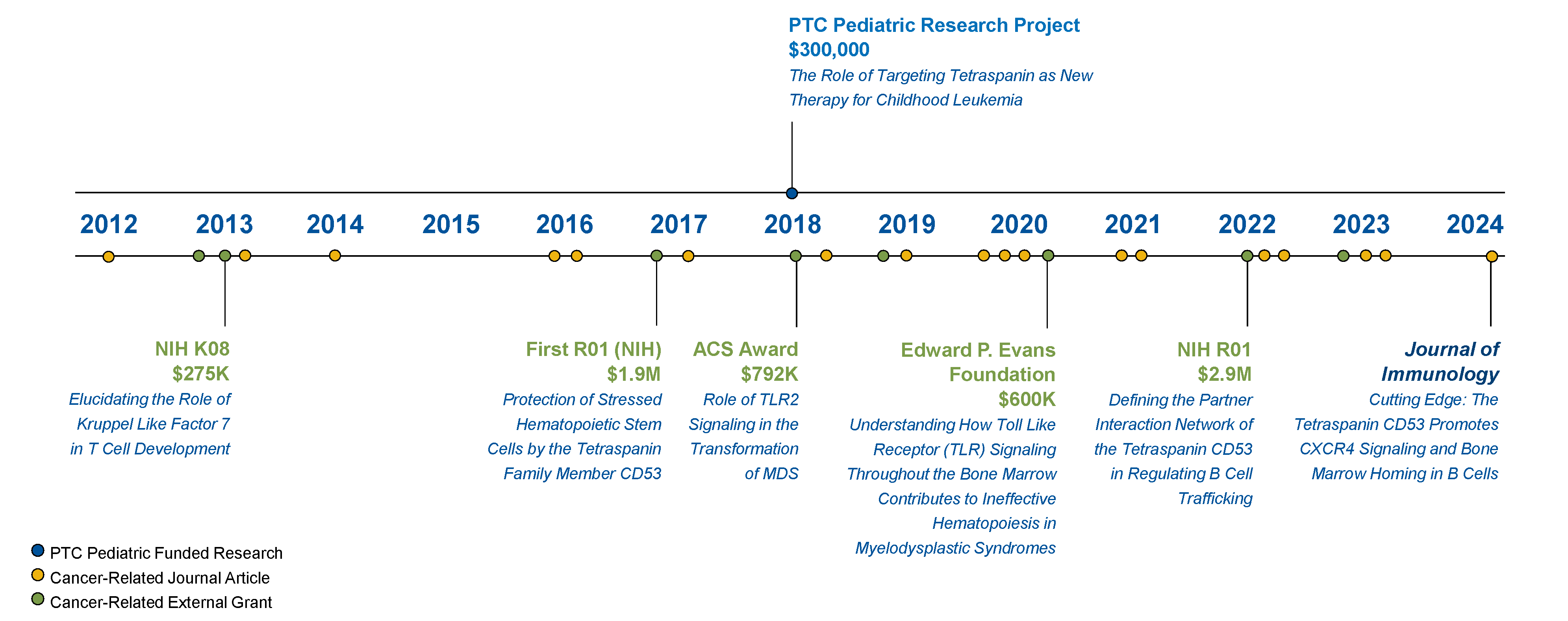
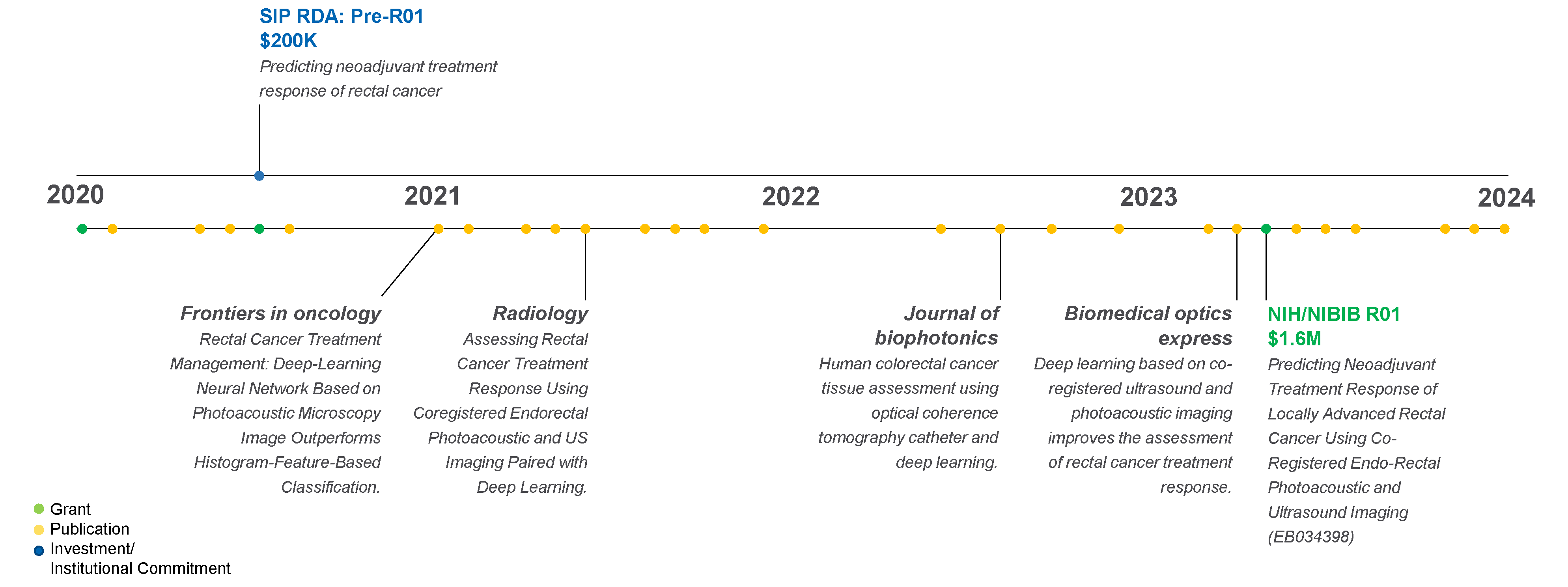
See how Pedal funds have spurred over half a billion dollars for cancer research in these research project investment timelines!
2025 Funded Research
Principal Investigator: Hyun Kim, MD
Co-PI's: Patrick Grierson, MD, PhD, and David DeNardo, PhD
Goal: This is a phase II, single-institution, open-label trial treating patients with borderline resectable (difficult to remove surgically) or locally advanced (cannot be removed by surgery) pancreatic cancer. The hypothesis is that advanced pancreatic cancer patients receiving treatment of adaptive (change the plan each day to adapt to patient’s anatomical changes in bowel and tumor position) stereotactic body radiotherapy (SBRT) plus defactinib + avutometinib at the same time will have more time after treatment during which the cancer will not progress (otherwise known as increased progression-free survival, or PFS) compared to historical PFS rates for patients receiving adaptive SBRT alone.
Description: Pancreatic ductal adenocarcinoma (PDAC) has a five-year survival rate of 12%. The only potential for a cure is surgical removal of the tumor (resection). However, despite 48% of patients presenting with advanced non-metastatic disease, only 10-15% of these patients are surgically resectable. Current standard of care for these locally advanced PDAC (LAPC) patients who are surgically unresectable is chemotherapy followed by consolidation stereotactic body radiation therapy (SBRT). However, more than half of these patients will progress to metastatic disease in one year. Current SBRT strategies infrequently generate sufficient tumor regression to enable a surgical option in LAPC patients. Thus, more effective treatment strategies for LAPC that lead to greater prevention of metastatic disease would directly improve PDAC patient survival. This application seeks to build on exceptional scientific, pre-clinical, clinical and biomarker findings. We will conduct a phase I/II study of SBRT plus FAK inhibition (Defactinib) and a RAK-MEK inhibitor (Avutametinib) in advanced pancreatic cancer patients. Our hypothesis is that this combination will be safe and lead long-term survival through modulation of tumor-intrinsic and immune pathways.
Principal Investigator: Stephen Oh, MD, PhD
Goal: This study investigates a new approach to treating certain types of blood cancers. Currently available treatments for these blood cancers are only partially effective. Thus, there is a desperate need to develop more effective treatments for these diseases. The proposed study involves the repurposing of a treatment that is currently in development for breast cancer. This would be the first study of this treatment in blood cancers. This study hypothesizes that PMD-026, an oral inhibitor of ribosomal protein S6 kinase A1 (RSK1), is safe and well tolerated in participants with MF and MDS/MPN and will improve spleen response, symptom response and bone marrow histopathological response.
Description: Myelofibrosis is a chronic myeloproliferative neoplasm (MPN) characterized by anemia, enlargement of the spleen, bone marrow fibrosis, fever, night sweats, fatigue and weight loss. Life expectancy with MF is limited, with a median survival of only five years. MF exhibits a propensity for transformation to post-MPN secondary acute myeloid leukemia (sAML), for which the prognosis is dismal (median survival < 6 months). Despite vigorous research, therapies capable of effectively treating MF and preventing progression to sAML remain elusive. Thus, there is a pressing need to develop novel therapeutic strategies for patients with these diseases. We initially identified aberrantly increased expression of the phosphatase DUSP6 in CD34+ hematopoietic stem/progenitor cells (HSPCs) from patients with MPNs transformed to sAML. Genetic and pharmacologic inhibition of DUSP6 inhibited MPN cell proliferation and suppressed downstream signaling effectors including phosphorylated RSK1 (pRSK1). To further understand the role of RSK1 (encoded by RPS6KA1), we performed patient-derived xenograft (PDX) experiments with sAML patient CD34+ HSPCs subjected to RPS6KA1 shRNA knockdown. Remarkably, RPS6KA1 knockdown led to near complete elimination of human CD45+ cells in the peripheral blood and bone marrow of engrafted mice. Our clinical trial challenges current treatment paradigms by investigating therapeutic targeting of a novel signaling pathway in myeloid malignancies. This investigator-sponsored study will be the first study with PMD-026 in blood cancers. The study additionally incorporates laboratory correlative studies (RNA-sequencing, mass cytometry, multiplex cytokine profiling, molecular genomics) to characterize how treatment with PMD-026 impacts downstream signaling effectors, inflammatory markers, and molecular response. This proposal leverages novel scientific concepts to address important unmet needs for patients with myeloid malignancies.
Principal Investigator: Sidharth Puram, MD, PhD
Co-PI: Douglas Adkins, MD
Goal: To reduce the dose of radiation and chemotherapy a patient receives after undergoing surgery for human papillomavirus (HPV)-related oropharynx squamous cell carcinoma (throat cancer).
Description: Despite improvements in operative techniques (e.g. transoral robotic surgery, or TORS), which have reduced short-term surgical morbidity for HPV+ oropharyngeal squamous cell carcinoma (OPSCC), otherwise known as throat or tonsil cancer, radiation and chemo after surgery remain a cause of significant long-term morbidity. While surgery is well-tolerated, post-surgery therapy often causes serious acute and chronic adverse events (AEs), including debilitating inflammation of the mucous membranes that line your mouth and GI tract, severe dry mouth, taste disorders and neck fibrosis/scarring among others, potentially resulting in long-term dependence on a feeding tube. Given the overall high rates of cure for HPV+ throat or tonsil cancer, there has been a strong focus on de-escalation of chemoradiation therapy (POACRT) in these patients to improve long-term morbidity. Our prior MINT trial (MINT-1) was a major step forward in de-escalation of HPV+ OPSCC patients. We believe this new proposal will significantly alter the standard of care adjuvant therapy of HPV+ throat and cancer patients and improve the therapeutic potential of current treatments. Importantly, MINT-1 was a non-randomized study; thus, at a minimum, confirming and extending the results of that study through MINT-2 represents a critical advance that is likely to yield adoption of this approach nationally and change the standard of care.
Principal Investigator: Lee Ratner, MD, PhD
Co-PI: Thomas Odeny, MD, MPH, PhD
Goal: This is a phase II, open-label, multicenter, single-arm treatment trial evaluating the use of propranolol (a beta blocker) to treat Kaposi sarcoma (KS), a disease in which cancer cells are found in the skin or lymphatic or visceral sites in the body. The hypothesis of this study is that an overall response rate (ORR = CR + PR rate) of at least 45% (as assessed by the AMC KS response criteria) will be achieved in participants, and that propranolol will be safe and well-tolerated by patients with KS. Our goals are to determine: 1) the safety and response of propranolol for KS, and 2) the effect on KS-associated gene expression.
Description: Infectious agents cause 20% of cancers worldwide. Kaposi sarcoma (KS) is caused by the KS γ-herpesvirus (KSHV). KSHV is also associated with primary effusion lymphoma, a B cell lymphoproliferative, preneoplastic disease, multicentric Castleman’s disease (MCD), and KS inflammatory cytokine syndrome (KICS). Treatment of KS involves immune reconstitution and/or systemic liposomal anthracyclines, taxanes, pomalidomide, or immune checkpoint inhibitors, but most of these therapies are not available low-income countries, and KS is one of the most common cancers in sub-Saharan Africa in HIV-negative or positive individuals.
Although remissions are obtained in most patients, complete remissions are rare, and continuous therapy is required. Propranolol is an inexpensive, globally available beta blocker, which is highly effective therapy for infantile hemangioma, and other vascular lesions and anecdotal reports describe successful treatment of KS with oral propranolol. Therefore, it is logical to assess the safety and activity of propranolol in a prospective clinical trial, and identify biomarkers of response. Single cell transcriptomics (scRNAseq) provides in-depth data about KS interactions with the tumor microenvironment, which will be utilized with baseline and on-treatment biopsies. We are uniquely qualified for this project given our extensive KS biological, pathological, epidemiological, translational and clinical experience.
Up to 25 eligible patients will be enrolled in a 2-stage phase 2 clinical study (18 at Washington University and 7 at the Kenya Medical Research Institute), with different KS subtypes, and treated with up to 20 weeks of propranolol. Successful completion of this study trial may provide a new, inexpensive, well-tolerated, globally available therapy for KS, and identification of biomarkers of response. This should prompt an assessment of beta blockers in other malignancies.
Principal Investigator: Todd Fehniger, MD, PhD
Project Leads: Carl DeSelm, MD, PhD; Robert Schreiber, PhD; Nathan Singh, MD, MS
Goal: The Cancer Immunity Team Science group is a translational, interdisciplinary research program with the overarching goal to develop new forms of immunotherapy that enhance a patients’ anti-tumor T cell immunity by design and thereby improve clinical outcomes or achieve cure.
Description: The Cancer Immunity program is a group of physicians and scientists united in the goal of discovering new strategies that initiate or promote a patient’s own T cells to destroy their cancer. These discoveries will then be translated into multiple novel treatment strategies that may have a broad impact on multiple cancer types. The projects utilize solid tumor (sarcoma) and blood cancer (lymphoma) immunocompetent mouse models to evaluate these new ideas, with translational relevance enhanced by confirming findings within lymphoma patient samples. The first project established these two cancer models in mice, defined key cancer cell proteins (neoantigens) targeted by T cells, developed neoantigen vaccines to initiate cancer immunity, and discovered a new CD4+ Tr1 cell that suppresses effective CD8+ T cell responses to these malignancies. This project serves as an integrative hub for the other projects. A second project investigates how chimeric antigen receptor (CAR) T cells bring about cancer immunity, and correlates key findings in samples from patients undergoing CAR T cell therapy. The third project defines the ability of CAR natural killer (NK) cells to increase anti-tumor immunity by enhancing neoantigen release via direct killing, dendritic cell localization and maturation, antigen presentation and T cell localization. Concepts discovered will be confirmed in humanized mouse models. The fourth project advances CAR dendritic cells, evaluating mechanisms to promote robust cancer immunity through epitope spreading, and combining with strategies that target suppressive cells, including Tr1 cells. The projects are highly integrated by evaluating Tr1 cells in each strategy, performance of inter-project experiments to address resistance to a single immunotherapy, and have shared model profiling that evaluates Tr1, T cells, NK cells and DCs across projects. The projects will be supported by research cores that facilitate uniform immunology and informatics analysis, biostatistics and shared mouse modeling, in a planned extramural team science program application.
Principal Investigator: Remco Bastiaannet, PhD
Co-PI: David Bauer, PhD (MU)
Collaboration with University of Missouri - Columbia
Goal: This proposal aims to develop a safer, more effective radiotherapy treatment for patients with advanced colorectal cancer that has spread to the abdomen — helping improve both survival and quality of life.
Description: Colorectal cancer often spreads to the lining of the abdomen, forming small tumors called peritoneal metastases. These tumors are especially hard to detect and treat and current therapies like systemic chemotherapy offer only limited benefit. There is a critical need for more effective and targeted treatments. This project explores a promising new strategy called intraperitoneal targeted alpha therapy (IP TAT). This approach delivers powerful cancer-killing radiation — known as alpha particles — directly into the abdominal cavity, where it can precisely target cancer cells while minimizing damage to healthy tissue. Alpha-emitters deliver extremely potent radiation and are increasingly being used in cancer patients, often successfully treating tumors for which other therapies have failed.
In the first part of this study, we will test a group of specially designed radioactive drugs that are made to seek out and attach to colorectal cancer cells. These agents are developed by our collaborators at the University of Missouri, who bring expertise in radiochemistry and tumor biology. By comparing different versions, we aim to find the one that most effectively reaches and sticks to tumors and stays in place long enough to be effective. In the second part of the project, we will use advanced imaging techniques and computer modeling—developed by the physicists and radiobiologists of the Washington University team — to precisely measure where the radiation accumulates and how much radiation the tumors receive. This will help us determine how best to eliminate cancer cells while avoiding harmful side effects.
Principal Investigator: Carmen Bergom, MD
Goal: The primary objective of this proposal is to investigate how cellular processes, such as autophagy and the activation of specific metabolic pathways, may enhance the effects of radiation therapy on tumors and protect the heart from radiation-induced damage. Our goal is to develop treatments that improve radiation’s helpful effects on cancer and reduce its harmful effects on the heart.
Description: Radiation therapy (RT) is an important component of modern cancer treatment; it is received by over half of all patients with cancer. Despite recent advances, RT does not cure all patients, and some experience harmful side effects — especially to the heart when the chest is treated. This highlights the need for new strategies to improve RT. We recently demonstrated that intermittent fasting (IF), a dietary approach that alternates periods of fasting with normal eating, enhances RT’s ability to kill tumors and also protects against RT-induced heart damage in animal models. IF can cause a wide range of effects, including increased cycling of a process called autophagy, which is linked to health and aging, as well as altered tumor metabolism. Our preliminary data from pre-clinical laboratory models suggest that IF and RT alter autophagy in tumors and the heart, which may lead to the favorable effects of combining IF and RT. Our metabolomics and other data from pre-clinical models suggest that regulation of branched-chain amino acid metabolism may also mediate the enhanced anti-tumor effects of IF on radiation. Our objective in this proposal is to use innovative preclinical techniques to determine how IF and RT impact autophagy and branched-chain amino acid metabolism in preclinical models of cancer and heart damage using RT. Our findings have the potential to identify translatable interventions that replicate the beneficial effects of IF, thereby enhancing radiation outcomes in patients with cancer. For instance, approved drugs used for other conditions may mimic IF, potentially improving RT efficacy in patients. These studies may lead to clinical trials and ultimately improved outcomes for patients with cancer.
Principal Investigator: Paul de Figueiredo, PhD (MU)
Co-PI: Milan G. Chheda, MD
Collaboration with University of Missouri - Columbia
Goal: The long-term goal of this project is to develop a new treatment for glioblastoma (GBM) by leveraging the immune-boosting effects of a safe and weakened version of a bacterium, Brucella melitensis, which we call SPIKE1.0.
Description: A major challenge in the treatment of patients with GBM is that patients’ immune systems do not attack the tumor. The tumor suppresses the number and function of immune cells around it. Researchers from the laboratories of Drs. de Figueiredo (University of Missouri) and Chheda (Siteman Cancer Center/Washington University) are working together on a new strategy using a safe, genetically modified bacterium that carries activating molecules, to lure and unleash anti-tumor defenses to attack and clear the tumor. Before moving to treatment in humans, they will rigorously test the hypothesis that this new treatment will improve the anti-tumor immune response in mice bearing brain tumors and significantly increase their survival. Upon successful completion of the specific aims of the project, the investigators will have the necessary preliminary data for an R01 proposal in which they will delve deeper into how this treatment works and develop even better therapeutic interventions. If successful, this research will eventually lead to a new treatment for glioblastoma patients that will improve their quality of life and help them live longer.
Principal Investigator: Aimee James, PhD, MPH
Goal: To change practice, increase lung screening, and reduce the elevated rates of lung cancer mortality in rural southern Illinois.
Description: Many rural communities, including those in the Siteman catchment area, experience persistently elevated rates of cancer and cancer mortality compared to more urban areas. This holds true for lung cancer. Low-dose CT (LDCT) scans are recommended for adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years. Less than 1 in 5 eligible adults are up to date with lung cancer screening, and rates are lower in rural areas. Rural southern Illinois is no exception to this trend and has areas that are health professional shortage areas and experience longer distances to care, persistent poverty and higher rates of tobacco use. We must find effective ways to increase lung cancer screening rates. Our team collaborated with Southern Illinois Healthcare, a rural health system, to develop, implement, and test a bundle of multi-level interventions (a “toolkit”) to increase colon cancer screening. We successfully partnered with providers to distribute patient education, deliver provider nudges, make systems changes and, and provide community awareness. In clinics that participated in the intervention, the likelihood of patients being screened for colon cancer was increased. We now propose to collaborate similarly to increase lung cancer screening. To transition this work to a successful NCI R01 trial, our toolkit must be substantially revised. As such, for this pre-R01 Siteman Investment Program study, we propose: Aim 1 — Identify primary care providers’ challenges in lung screening and preferences for intervention support. We will conduct interviews and site visits at primary and specialty care, to examine the context and challenges of lung cancer screening and identify provider-proposed strategies to increase screening. We will interview patients to identify potential areas of hesitance or needs for support. Aim 2 — Build on prior work and Aim 1 findings to create a toolkit to help primary care providers increase lung cancer screening. We will adapt our existing materials, while bringing in new LDCT specific elements. Aim 3 — Prepare for successful R01 by completing two key foundational steps: (1) Begin adaptation of health maintenance page in EHR to make screening easier to find and (2) add lung cancer screening materials to SIH’s community outreach. We will observe and investigate perceptions of these materials for improvement in our trial. This work is necessary for our future R01 and will directly lead to a stronger NCI application. Our likelihood of success with NCI funding is better if we have developed these components, which we feel we can do with this SIP research. We plan to submit the R01 in 2026.
Principal Investigator: Christopher Malone, MD
Goal: To identify predictive biomarkers of treatment response and resistance, supporting future precision strategies to optimize the use of Y-90-RE and ICIs in early and intermediate stage hepatocellular carcinoma, a type of liver cancer.
Description: Hepatocellular carcinoma (HCC) is a leading cause of cancer-related death globally, with increasing incidence in the United States driven by metabolic-associated steatotic liver disease (MASLD, or fatty liver disease) and alcohol-related liver disease. While Yttrium-90 radioembolization (Y-90-RE) is a highly effective liver-directed therapy capable of achieving complete tumor response in early-stage HCC, a substantial proportion of patients, particularly those with more advanced disease, experience recurrence due to minimal residual disease (MRD). This failure to eradicate all viable tumor cells is likely driven by underlying differences between tumor cells, such as the presence of treatment-resistant cancer cells and the ability to avoid detection by the immune system. Although immune checkpoint inhibitors (ICIs) have shown promise in advanced-stage HCC, their use in early and intermediate HCC stages in combination with Y-90-RE is currently empirical and lacks molecular guidance. This proposal aims to identify molecular and tumor immune microenvironment (TME) features associated with response or resistance to Y-90-RE, and to determine which patients may benefit from the addition of ICIs. Using a unique biobank of pre-treatment biopsies and explant specimens from HCC patients treated with Y-90-RE with or without ICIs, we will analyze how genes are active in different parts of the tumor using advanced spatial mapping technology called Xenium.
Principal Investigator: Nima Mosammaparast, MD, PhD
Co-PI: Hani Zaher, PhD
Goal: To understand the workings of a specific pathway (RNF113A-ASCC) that maintains genome stability and is lethal to cells with the c-Myc oncogene, a gene that plays a crucial role in cell growth and cancer proliferation.
Description: The main goal of this proposal is to understand the mechanism of a specific pathway that maintains genome stability and is lethal to cells with the c-Myc oncogene, a gene that plays a crucial role in cell growth, proliferation, and cancer metabolism. Our team discovered a new signaling pathway that starts when cells face damage to their DNA and RNA bases, a common effect of cancer treatments. This pathway involves two key proteins, RNF113A and SMYD3, which help bring repair enzymes to the damaged DNA. We’ve found that RNA signaling is crucial for activating this repair pathway. Our findings suggest that a certain protein (known as ASCC3 helicase) helps separate the spliceosome from the DNA, which is important when there’s increased stress from high c-Myc activity. We believe this pathway works during active RNA transcription and processing, which makes targeting it in tumors with high c-Myc levels a promising strategy. In this proposal, we plan to inhibit the RNF113A-ASCC pathway using genetic tools and existing drugs that act as inhibitors of SMYD3 to see if it can effectively fight small cell lung cancer (SCLC), a deadly cancer often linked to c-Myc amplification. We will also study how this pathway helps manage stress from high transcription to prevent harmful DNA-RNA structures and replication issues (Aim 2). This research aims to enhance our understanding of genome stability and its application in cancer treatment.
Principal Investigator: David Spencer, MD, PhD
Goal: To define the changes in DNA methylation (chemical changes in DNA) that occur in acute myeloid leukemia and leverage these insights to improve our understanding of the way the disease forms and our ability to predict its potential return after treatment.
Description: Acute myeloid leukemia (AML) is a lethal hematologic malignancy characterized by mutations in hematopoietic (blood) stem cells. Prior research has shown that AML can develop from pre-existing clonal bone marrow diseases, including clonal hematopoiesis (CH) and myelodysplastic syndromes (MDS), and there is extensive overlap in the mutational spectrum across these conditions. In some CH and MDS patients, transformation to AML can occur with little change in the genetic composition of the cancerous cells, indicating a role for other contributing factors. DNA methylation is a chemical change in DNA that is essential for normal tissue development and is universally abnormal in AML patients. Recent studies by our lab have used new methods to directly sequence native DNA molecules without modifying them first, which improves our ability investigate changes in DNA methylation as a potential source of novel contributing factors to AML development. This approach identified specific regions in the DNA of patients with AML where DNA methylation was different between the maternal and paternal copies of specific genes that are important for blood cell function. These methylation patterns stayed the same in samples from the same patients at the start of their illness as when the illness came back, and they were also seen in these patients when they did not have active disease but still had signs of cancer cells based on genetic tests. Many of these “methylation spots” were recurrent across multiple patients and affected how easily parts of the DNA could be accessed, and they affected genes that control how stem cells grow and renew themselves, including a gene called GATA2 that is known to be very important for blood cell development.
Based on this evidence, we hypothesize that specific changes in DNA methylation represent clonal “epimutations” that can disrupt normal gene regulation and be selected for during the formation of leukemia. We further hypothesize that epimutations create a unique pattern in leukemia cell populations, which means they could help detect leftover leukemia cells when patients are in remission. In this proposal, we will study how DNA methylation epimutations affect the GATA2 gene by closely examining the structure of the chromatin in leukemia cells. After that, we will create a new testing method to detect both genetic mutations and these epimutations. This test will help us find remaining leukemia cells in patients who seem cured after chemotherapy. Overall, these studies will help us understand how DNA methylation epimutations impact the GATA2 gene in leukemia and offer new strategies for improving early detection, monitoring, and treatment of disease relapse.
2024 Funded Research
Principal Investigator: Russell Pachynski, MD
Co-PI: Daniel Thorek, PhD
Goal: To determine the recommended phase 2 dose of an immunotherapy treatment for metastatic castrate-resistant prostate cancer that combines a protein called N-803 with a Food and Drug Administration (FDA)-approved cellular immunotherapy called sipuleucel-T (Provenge). Researchers hypothesize that the combination will have an acceptable safety profile and will be feasible to administer in this population.
Description: Immunotherapy is an emerging treatment platform for cancer patients that can be highly effective. However, only a subset of patients demonstrates long-term responses. A persistent challenge has been how to identify patients that would benefit, and how to enhance immunological treatments to benefit more patients. This proposal addresses these critical issues by:
- Combining two immunotherapies that the researchers have shown work together in preclinical models
- Advancing a promising functional scanning technology to noninvasively characterize the immune response in these patients
Prostate cancer is the second most diagnosed cancer in males. Surgery or radiation can be curative when treated early and localized to the prostate; however, it is incurable once it has spread. Novel modes of treatment are needed. The researchers propose to combine Sipuleucel-T, an FDA-approved adoptive cell therapy for prostate cancer with modest outcomes, with N-803, an immunostimulatory engineered protein that binds to interleukin-15, a cytokine involved in activating immune cells. N803 has recently been FDA-approved for bladder cancer. The researchers will establish optimal dose and schedule for this new combination approach across three treatment cohorts. They will study the immune responses in blood, and use novel, functional noninvasive imaging of the active immune system using a novel radiotracer (specific for an immune mediator called granzyme-B). Together, this work is immediately impactful to men with prostate cancer and expands the horizons for the improved understanding of how the immune system responds to and may guide treatment.
Principal Investigator: Nicole Brossier, MD, PhD
Goal: To improve the outcomes for brain tumors in children. This proposal aims to determine how different dietary components (fat and sugar) affect tumor formation, epidermal growth factor (EGF) levels and epidermal growth factor receptor (EGFR) signaling in a murine model of pediatric brain tumor formation, and then to determine whether inhibition of EGFR prevents diet-accelerated tumor formation in this model. This information will be used to improve dietary counseling in patients and to design subsequent studies testing the benefits of risk-adapted therapeutic strategies in children with brain tumors and poor dietary exposure.
Description: As we enter into an era of precision pediatric oncology, it is becoming increasingly important to identify the factors that underlie the risk of brain tumor development. This challenge is particularly relevant for individuals with cancer predisposition syndromes like NF1, where 15-20% of children born with a germline NF1 gene mutation develop optic pathway gliomas (OPGs). Our inability to provide accurate risk assessment information for these young children leads to frequent sedated neuroimaging, suboptimal visual screening and delays in instituting treatment for those at greatest risk. The researchers recently performed pre-clinical studies that found exposure to an unhealthy, obesity-promoting diet (obesogenic diet, Ob) increased the likelihood of OPG development in NF1 mouse models. They also identified that these animals have much higher levels of epidermal growth factor (EGF) in their blood. Based on these observations, as well as findings that a high-fat diet drives tumor formation in other tumor types through activation of the EGF receptor (EGFR), the researchers hypothesize that high dietary fat intake drives NF1-OPG formation through increased EGFR signaling. In this grant, they propose to perform a detailed analysis of how different diets (high-fat, high-sugar or high-fat, high-sugar) affect NF1-OPG formation and how this correlates with circulating EGF levels. They will then inhibit EGFR through genetic and pharmacologic means in Ob-diet-driven NF1-OPG to determine whether this impairs tumor formation. Taken together, these experiments will determine how dietary composition affects tumor formation and the role of EGF in this process. This will provide a foundation for future investigations to determine whether EGF may be used as a biomarker to detect children at higher risk of NF1-OPG due to dietary exposure and to ascertain whether EGFR-directed therapy could be a useful addition to the existing treatment strategy of NF1-OPG in children with poor diets.
Principal Investigator: John DiPersio, MD, PhD
Goal: To improve anti-CD19 chimeric antigen receptor T cell (CART19) therapy for patients with relapsed or refractory large B-cell lymphoma (r/r LBCL). Currently, long-term disease-free survival with commercial CART19 in r/r LBCL is only about 40%, so more strategies to improve the efficacy of CART19 are warranted.
Description: Diffuse large B-cell lymphoma (DLBCL) is a common type of fast-growing non-Hodgkin lymphoma. In about 33% of patients, DLBCL returns after the first treatment (relapsed DLBCL), or the first treatment is not effective and the patient is not cured (refractory DLBCL). The FDA has approved three chimeric antigen receptor T-cell (CAR-T) therapies for use in adults with relapse or refractory DLBCL. T cells are a part of the immune system and help protect the body from infection and cancer. CAR-T therapy involves engineering healthy T cells to attack cancer cells. Unfortunately, about 50% of patients treated with CAR-T cells will relapse again with DLBCL within eight months. Interleukins are a type of protein that help activate our immune system to fight infections and cancer. Three interleukins named IL-7, IL-15, and IL-21 are especially effective at helping T cells survive, proliferate and kill infected cells. In this proposal, the researchers are testing if IL-7, IL-15 and IL-21 can help CAR-T cells kill DLBCL. Since interleukins are very short-lived and only last for one to two hours, they are testing novel long-acting versions of IL-7, IL-15 or IL-21 that last two to three days in humans. In part 1 of their proposal, the researchers are performing a clinical trial to determine if a drug named NT-I7, which is a long-acting version of IL-7, is safe and effective in helping CAR-T cells kill DLBCL tumors. In part 2, they are testing a new compound named HCW9206 that merges IL-7, IL-15 and IL-21 into a single long-acting drug. Their studies with HCW9206 will test its safety and ability to help CAR-T cells kill DLBCL in mice.
Principal Investigator: Yoon-A Kang, PhD
Goal: To identify a treatment for a broad range of myeloproliferative neoplasms (MPNs) independent of individual mutations. This project will focus on cells called multipotent progenitor 3 (MPP3), the expansion of which are common in a range of MPNs, and will investigate whether the process of controlling MPP3 blood cell production mechanisms can be targeted to regulate the excessive production of myeloid cells and form the foundation of a future therapy.
Description: Myeloproliferative neoplasms (MPNs) are a group of diseases characterized by too many white blood cells, red blood cells or platelets in the bone marrow. There are several well-known disease-causing mutations, and researchers have targeted these mutations to develop treatments. Although targeted therapies have revolutionized MPN treatment, they are not curative in most cases as the mutant cell population driving disease development and recurrence is usually not eradicated. However, their success in controlling disease development and progression has shown the clinical importance of normalizing blood production in disease contexts. Additionally, there are patients without known driver mutations, with no targetable driver mutations or who develop resistance to targeted therapies. Therefore, a better understanding of the mechanisms underlying myeloid cell expansion, a shared feature of various MPNs, is necessary to develop new treatments to be used in combination with current targeted therapies or as alternatives for patients who are ineligible for current therapies. The goal of this study is to find a treatment that is applicable to a broad range of MPNs independent of individual mutations. The researchers’ previous work found there is a specific immature bone marrow population, called multipotent progenitor 3 (MPP3), that can generate white blood cells, red blood cells and platelets. Importantly, MPP3 is expanded in various MPN mouse models regardless of their driver mutations. Interestingly, distinct MPP3 subsets are specifically increased corresponding to the overproduced mature cell types in MPNs. This indicates that controlling the production of different MPP3 subsets can regulate disease development and progression irrespective of disease-causing mutations. For this project, the researchers propose to study two commonly dysregulated pathways in human blood malignancies to control the production of distinct MPP3 subsets. Their study will provide insights into the common mechanism underlying MPN development and foundations to develop broadly applicable therapeutic interventions.
Principal Investigator: Kiran Mahajan, PhD
Co-PI: Nupam Mahajan, PhD
Goal: To demonstrate that a protein called HOXB13 can be targeted to treat prostate cancer with novel combination therapies. The study will benefit African American patients expressing increased HOXB13 through genetic and epigenetic mechanisms.
Description: Prostate cancer disproportionately affects African American men compared to white men. Recently, a HOXB13 variant (X285K) predisposing to prostate cancer in men of West African ancestry was reported in a large-scale germline genetic testing. HOXB13-X285K was significantly enriched in self-reported Black (1.01%;~21000 men screened) versus white (0.01%) patients. HOXB13-X285K carriers tended to have more aggressive disease, due to increased protein stability that resulted in an increase in cell proliferation. Besides germline mutations, gain-of-function modification in HOXB13 bump up HOXB13 RNA and protein levels. Thus, screening for HOXB13 expression and development of effective treatments is critical to improve clinical outcomes. Prostate-Specific Membrane Antigen-Targeted Imaging (PSMA-PET) imaging could be combined with molecular profiling of prostate biopsies for HOXB13 expression in white and African American patients for early detection and treatment of aggressive prostate cancers.
Results from this study will reveal previously unknown epigenetic regulation of immune suppression in prostate cancer. The researchers’ pre-clinical studies will advance the use of other checkpoint inhibitors alone or in combination with PD-L1/PD-1 axis to overcome poor response to immunotherapy. The results will provide the basis for combination therapies to improve treatment outcomes for prostate cancer patients.
Principal Investigator: Laura Schuettpelz, MD, PhD
Goal: To determine how the gene called Stathmin 1 (Stmn1) regulates hematopoietic stem cell (HSC) metabolism and contributes to hematopoietic malignancies, especially leukemia. The researchers predict that high levels of Stmn1 support the needs of growing leukemic cells, and that it may be a new therapeutic target on which to focus.
Description:The gene stathmin 1 (Stmn1) is expressed at high levels in normal blood stem cells and is overexpressed in blood cancer cells. The researchers’ preliminary studies suggest that Stmn1 is important for supporting various aspects of healthy blood stem cell metabolism, including maintaining healthy mitochondria and protein turnover in the cell. They predict that high levels of Stmn1 in leukemia cells are necessary to sustain the unique metabolic needs of leukemia cells. The proposed studies will determine the mechanisms by which Stmn1 influences blood stem cell metabolism, and in future studies researchers will determine whether inhibition of Stmn1 impairs the growth of leukemic blood cells. Ultimately, these studies will test Stmn1 as a novel therapeutic target to treat leukemia. As Stmn1 is overexpressed on multiple types of blood cancers, and loss of Stmn1 in mouse models has few effects outside of the blood system, the researchers predict that Stmn1-directed drugs could be useful to treat a wide variety of leukemias with limited side effects.
Principal Investigator: Stephen Sykes, PhD
Goal: To identify molecular pathways that support chemotherapy resistance in acute myeloid leukemia (AML) and utilize that information to identify potential new therapeutic targets. This proposal will specifically focus on a protein called DNA-Damage Induced Transcript 4 (DDIT4) that the researchers hypothesize supports AML cell survival and chemotherapy resistance and will establish that targeting this protein in a certain pathway will have therapeutic potential for leukemia patients.
Description: Annually, approximately 1 in 12,500 Americans are diagnosed with acute myeloid leukemia (AML), and more than 12,000 die from the disease. The overall survival rate of AML patients is below 25% for adults and 70% for children, and these poor outcomes are largely due to high rates of resistance to the current standard-of-care treatments and disease relapse. The researchers have discovered that a protein called DDIT4 (DNA-Damage Induced Transcript 4) may play a central role in how AML cells evade current chemotherapies. This project will decipher the molecular mechanisms by which DDIT4 promotes chemotherapy resistance as well as test whether pharmacological targeting of DDIT4 enhances the anti-leukemia effects of current chemotherapies.
Principal Investigator: Alessandro Vindigni, PhD
Co-PI: Sergej Djuranovic, PhD
Goal: To study early detection strategies for breast and ovarian cancer in women with BRCA1 or BRCA2 gene mutations and research molecularly guided and nonsurgical interventions to prevent tumor development.
Description: More than 1 in 500 women are affected by mutations in the breast cancer susceptibility genes BRCA1 or BRCA2. While it is known that these women have up to an 80% risk of developing breast and ovarian cancer in their lifetime, exactly why these cells become cancerous is unknown. The only preventive options currently available are risk-associated prophylactic surgeries of ovary/fallopian tube and breast removal, which result in surgical menopause and significant aesthetic consequences. Therefore, two major challenges that women with BRCA1 or BRCA2 gene mutations currently face are the lack of:
- Early detection strategies to identify which carriers will develop these malignancies
- Molecularly guided and nonsurgical strategies to prevent breast and ovarian tumor development
This project joins experts in DNA replication (Alessandro Vindigni, PhD), RNA processing (Sergej Djuranovic, PhD), and ovarian cancer (Mary Mullen, MD, MSCI) to tackle these challenges. The researchers know that BRCA1 is important for DNA replication and it helps protect the genome. Women with mutations in the BRCA1 gene have less BRCA1 protein in their cells. The researchers believe this lack of BRCA1 protein causes problems with DNA replication. These problems lead to more mutations in the genome, which can cause cells to become cancerous. They will test these new ideas using fallopian tube cells, new technologies from the Vindigni lab, and samples from patients. Next, they will use a technology developed by the Djuranovic lab called “antisense oligonucleotides” to increase BRCA1 protein levels. The researchers think that by increasing this protein, they can stop the unstable replication forks and prevent mutations that cause these cancers. Collectively, their studies will:
- Define the early changes that happen when normal fallopian tube cells with BRCA1 gene mutations turn into tumors
- Establish novel nonsurgical strategies to prevent ovarian cancer development in women with BRCA1 gene mutations
Principal Investigator: Matthew Walter, MD
Goal: To begin developing a new way to treat patients suffering from myelodysplastic syndrome, or MDS, by understanding how blood cells with mutations grow and expand. This project will test the safety and efficacy of selectively eliminating mutated blood cells by hyperactivating a pathway that reduces their growth, which could improve patients’ lives.
Description: Myelodysplastic syndromes (MDS) are one of the most common types of blood cancer in adults. MDS patients suffer from problems related to low blood counts, including life-threatening infections and bleeding. Once MDS develops, the only cure is a bone marrow transplant. However, most patients are not eligible for a transplant due to their advanced age and other illnesses. Understanding how MDS develops may help researchers identify new ways to treat patients with MDS.
Up to half of MDS patients have mutations in genes in their blood cells that regulate how RNA is stitched together in a cell, called RNA splicing. A goal of this project is to understand how blood cells with a gene mutation that controls RNA splicing grow, expand and cause MDS. The researchers observed that early after a cell gets an RNA splicing gene mutation, mutant cells grow slower than normal cells. However, over time, a mutated cell changes and outgrows normal cells, causing MDS and other blood cancers. The researchers are studying what happens early after a mutation occurs in a blood cell so they can identify ways to kill cells with the mutation.
Their initial studies identified a pathway in mutant blood cells that they can hyperactivate to preferentially kill mutated cells in a culture dish. The researchers now want to test if they can kill mutant cells in preclinical models and see if it is safe. If this works, they could design a trial to test if a new approach could kill mutated MDS cells in patients and improve their lives.
Principal Investigator: Tanner Johanns, MD, PhD
Goal: To determine if adding an immune boosting agent, called a PD-1 inhibitor, to a personalized cancer vaccine improves immune responses in patients with newly diagnosed glioblastoma, the deadliest brain tumor in adults.
Description: Glioblastoma is the deadliest brain tumor in adults with limited treatment options. To date, therapies that aim to induce the patients' own immune response to cancer cells have not been effective in glioblastoma for unclear reasons. Understanding why immune therapies are ineffective and how to overcome these barriers is the primary focus of our laboratory. To this end, we recently completed a study targeting neoantigens, proteins derived from mutations unique to each patient tumor, using a robust discovery pipeline, called pVac-Seq, developed at Washington University. Neoantigens were incorporated into a DNA vaccine platform and administered to patients after completion of radiation. Preliminary results showed successful induction of immune responses to neoantigens after vaccination with some long-term survivors. Based on these encouraging results, this present study will combine personalized neoantigen DNA vaccines with another immune boosting agent, termed a PD-1 inhibitor, which is approved for treatment in other cancers but has not been effective in glioblastoma. The goal of this study is to determine if the combination of neoantigen vaccine with PD-1 inhibition improves the immune response to vaccine-encoded neoantigens in patients with newly diagnosed glioblastoma. Additionally, neoantigen vaccination in combination with PD-1 inhibition is being explored in more immune sensitive solid tumors like melanoma with the idea that induction of a neoantigen-specific immune response from the vaccine will improve response rates to PD-1 inhibition. Therefore, in addition to PD-1 inhibition improving the efficacy of the neoantigen vaccine, it is also possible that the administration of a neoantigen vaccine improves the response to PD-1 inhibition in glioblastoma. Together, we hope this combination therapy improves outcomes for patients with glioblastoma, and that the results of this study provide the necessary justification to continue developing this promising therapy for our patients with brain tumors, where there is a critical need for novel effective treatment options. Ultimately, if effective, we hope this combination therapy will be incorporated into the standard treatment regimen for patients with glioblastoma and serve as a backbone to explore other immune therapy strategies that could further improve outcomes in this patient population.
Principal Investigator: Maria Thomas, MD, PhD
Goal: To compare the toxicity and efficacy of 1 week of radiotherapy (SWIFT RT) versus 3 weeks of radiotherapy (RT) given to the breast and nodes, while also evaluating patient quality of life and breast cosmesis.
Description: For women with breast cancer which has spread to their lymph nodes, treatment often includes radiation (high energy x-rays focused on the breast and nodes to kill cancer cells which may have been left behind after surgery). This reduces the risk of cancer recurrence and improves a patient’s chance of surviving breast cancer. Traditionally, a course of breast cancer radiation required 5-6 weeks of daily treatments (Monday through Friday). Although each treatment takes about 15 minutes, daily appointments for 6 weeks can impact work, childcare, quality of life, and/or other obligations. Over time, shorter, more condensed courses of radiation (3 weeks) have been shown to be just as effective and just as well tolerated. When the 3 week schedule was studied in patients with cancer spread to the nodes, this was also effective and well tolerated. Recently, a trial called UK FAST FORWARD found that one week of radiation is just as effective and well tolerated, when compared to 3 weeks. However, in that trial, radiation was only given to the breast. Therefore, if cancer has spread to the nodes, 3 weeks remains standard. In this randomized trial (SWIFT RT), we will compare 3 week versus 1 week of radiation to the breast and nodes. Given this had excellent effectiveness and safety when given only to the breast, we expect similar results with the one week schedule in this trial. We will also evaluate patient quality of life and collect blood samples to study toxicities from treatment, in order to offer even more individualized patient care in the future. If one week of radiation to the breast and nodes is found to be effective and well-tolerated, this would be a huge impact for women with breast cancer and would improve worldwide access to care by reducing the length of treatment.
Principal Investigator: John Krais, PhD
Goal: To explore how DNA damage accumulates and is repaired in non-cancer cells carrying a BRCA1 mutation and address the exciting possibility that suppressing a DNA repair pathway called polymerase theta-mediated end joining (TMEJ) could eliminate the transformation of cells into a malignant state.
Description: Mutations in genes encoding the DNA damage response machinery, including BRCA1 and BRCA2, lead to a significantly elevated risk of ovarian and breast cancer development for individuals inheriting a mutant gene. Inheritance of a mutation from one parent is sufficient to trigger tumor formation, despite also receiving a functional, non-mutated (wild-type) gene copy from the other parent. These high-risk individuals, usually with a family history of cancer, are in dire need of new tumor prevention approaches. The development of cancer prevention strategies is precluded by a shockingly limited understanding of the process where normal cells undergo transformation to malignant cancers. In fact, cells with one wild-type and one mutant copy of the BRCA1 or BRCA2 genes demonstrate very mild differences, even in their DNA damage response capabilities, yet are susceptible to cancer development. To address this paradox, we developed a BRCA1 mutant transgenic mouse strain and derived cells with wild-type BRCA1 or a single mutant copy to recapitulate an inherited mutation. In preliminary experiments we found a subtle accumulation of DNA damage in cells with a mutant copy of BRCA1 but revealed a startling increase in the activation of a mutagenic backup DNA repair pathway, Polymerase Theta-mediated end joining (TMEJ). These potentially transformative results raise the possibility that TMEJ is responsible for the mutations (mutagenesis) required for tumor development. In this proposal, we explore how DNA damage accumulates and is repaired in non-cancer cells carrying a BRCA1 mutation and address the exciting possibility that suppressing TMEJ could eliminate the transformation of cells into a malignant state.
Principal Investigator: Stephanie Markovina, MD, PhD
Goal: To determine if small drug-like molecules can be designed to block the many protective effects that a certain protein called SERPINB3 has on cervical tumor cells, and whether this approach can sensitize cancer cells to chemoradiation therapy to a greater extent than normal cells to better treat the cancer while reducing the potential of treatment side effects.
Description: Cervical cancer is responsible for a large number of cancer deaths worldwide. The standard treatment is a combination of radiation and chemotherapy and has not changed for decades. Only recently have new treatments that stimulate the patient’s immune response against the cancer shown promise. These drugs, called immune checkpoint inhibitors (ICIs), appear to work well for a small proportion of patients, and which patients will benefit from the addition of this treatment is unknown. Additionally, why some patients do not respond to standard chemoradiation or ICIs is also unknown. We have discovered that a protein called SERPINB3 protects tumor cells from anticancer therapy. This protein appears to protect tumor cells directly by preventing cell death when treated with chemoradiation and other drugs, but also by influencing the immune cells within the tumor. Currently, there are no drugs that block the action of SERPINB3, and it is unclear if targeting SERPINB3 might also sensitize normal non-cancer cells to these therapies, increasing the risk of side effects. In order to address these gaps in knowledge, I propose two specific goals for this project: 1) determine if small molecules can specifically inhibit the protective effect of SERPINB3 on cervical tumor cells, and 2) if targeting of SERPINB3 sensitizes cancer cells to a greater extent than normal cells. To achieve these goals, we will employ novel tools we have developed to mimic conditions and treatments that are delivered to patients. Drug candidates we have identified through screening will be tested in these settings and fill the gap in knowledge about cervical cancer resistance and nominate new treatment approaches to improve survival from cervical cancer. While this proposal is focused on cervical cancer, the development of SERPINB3-targeting drugs may represent a personalized treatment approach for many patients with tumors that express SERPINB3, including lung cancer, head and neck cancer, and an aggressive brain tumor called glioblastoma, extending the reach of this research to an even greater number of patients.
Principal Investigator: Karla Washington, PhD
Goal: To enhance the well-being of the family caregivers of cancer hospice patients by implementing and evaluating modifications to the ENVISION digital health tool and conducting a rigourous feasibility pilot study.
Description: Each year, nearly half a million Americans with advanced cancer elect to receive hospice services when disease-directed therapies are no longer effective and life expectancy is limited. Most of these individuals receive hospice in the community with family members and friends managing their symptoms, often with little training or preparation. Symptom management challenges are common in hospice, and they are a significant source of patient and family caregiver distress. For the past several years, our team has worked with hospice providers and care recipients to co-create a digital health tool and corresponding intervention called ENVISION (ENgagement and Visualization to Improve Symptoms In ONcologic care). The ENVISION application converts patient- and family caregiver-reported symptom and well-being indicators into simple data visualizations, which are summarized in daily scorecards that provide hospice teams with comprehensive, yet easily interpretable assessment data to guide care planning and prioritization of clinical responses. We recently conducted an evaluation of ENVISION's digital inclusivity in preparation for a large, multi-site trial. Evaluation results highlighted two modifications that, if implemented, would significantly increase ENVISION's usablity and potential benefit for diverse groups of patients and family caregivers: (1) simplifying the onboarding experience to make it easier for users with low digital literacy to log in to the application the first time, and (2) providing additional training to help family caregivers assess patient symptoms, particularly in more advanced disease stages. In this application, we propose a two-year study that will allow us to implement and evaluate these modifications and conduct a rigorous feasibility pilot study. At the conclusion of the proposed research, our team will be well-positioned to pursue robust external support for a large-scale, multi-site clinical trial of ENVISON, which we hypothesize will decrease family caregivers' distress and improve management of patient symptoms in home hospice care.
Principal Investigator: Jingyu Xiang, MD, MSCI
Co-PI: John DiPersio, MD, PhD
Goal: To utilize a genetic tool called CRISPR to generate more effective CAR-T cell therapy against tumor cells and to generate healthy immune cells that are resistant to CAR-T cell attacks. This would promote the killing of T-cell acute lymphoblastic leukemia (T-ALL) cells while preserving the immune system.
Description: T cell acute lymphoblastic leukemia (T-ALL) is an aggressive blood cancer arising in T cells, an important component of the immune system. Patients with T-ALL who relapse have a poor prognosis, with a five-year survival rate of less than ten percent. Chimeric antigen receptor T cell (CAR-T) therapy is a promising treatment that involves engineering healthy T cells to attack cancer cells. However, the marker that CAR-T cells use to recognize and kill T-ALL is also expressed on themselves and other healthy immune cells. This causes CAR-T cells to attack each other (fratricide) or healthy immune cells, which leads to poor CAR-T function and immunodeficiency. In this study, we will develop a novel CAR-T therapy that targets CD2, a surface marker expressed on both T-ALL and healthy T cells. To prevent CAR-T cells from killing themselves and instead focusing on attacking cancer cells, we will use a genetic tool called CRISPR to mask the CD2 marker on CAR-T cells, so they are not recognizable by the CAR-T cells. By applying this genetic tool to hematopoietic stem cells, which give rise to all the cells in the blood, we can generate healthy immune cells that are resistant to unwanted killing by CAR-T cells, therefore preserving the immune system. We hope this novel immunotherapeutic approach will thus promote T-ALL killing while preserving a healthy immune system.
Principal Investigator: Jeffrey Magee, MD, PhD
Description: In collaboration with the McDonnell Pediatric Cancer Research Center (MPCRC), we have launched a funding initiative called “Amplification Awards” to ensure that highly meritorious pediatric cancer-related research is sustained to completion in the context of NIH funding cuts and rising research costs. The overarching premise is to supplement research projects that currently have NIH funding yet remain underfunded. These projects have already undergone rigorous scientific review and been deemed exceptional. However, they are at risk for not meeting their full potential – in terms of new knowledge and new therapies – because of budget cuts and rising overall costs.
While the MPCRC and the Division of Pediatric Hematology Oncology remain committed to funding new investigators and pilot research, as we have for a long time, the Amplification Awards meet an emerging need, especially for our talented mid-career faculty. They will ensure that the promise of successful pilot efforts goes fulfilled.
We have established a two-step review process under the auspices of the annual MPCRC funding cycles. The first stage involves a letter of intent to ensure eligibility. The awards are meant to amplify research that directly relates to childhood cancer and has successfully garnered NIH funding (or has received a clearly fundable score). The second stage involves review of progress to date on the funded aims. Since the proposals already have been deemed scientifically meritorious by the NIH, the internal review emphasizes accomplishment and relevance to pediatric cancer treatment. The MPCRC scientific advisory board oversees the review process. This year we anticipate funding 5 eligible investigators within the Division of Pediatric Hematology and Oncology.
Principal Investigator: Nicole Brossier, MD, PhD
Description: This project is funded in collaboration with Siteman Cancer Center. Children with the pediatric brain tumor predisposition syndrome Neurofibromatosis Type 1 (NF1) are at risk for low-grade gliomas in the optic pathway (optic pathway gliomas; OPGs). However, there is significant clinical heterogeneity in the presentation of these tumors, and we currently cannot predict which children will develop OPGs or how severe their clinical manifestations will become. Consistent with epidemiologic studies showing that maternal obesity is associated with higher rates of pediatric glioma formation, obesogenic (high-fat, high-sugar; HFHS) diet exposure has recently been shown to accelerate Nf1-OPG formation and increase tumor penetrance, in part through effects of maternal diet on the Nf1-OPG cell of origin. While neither the dietary component mediating this response nor its downstream effectors have been elucidated, Ob-exposed Nf1-OPG mice display significantly higher levels of EGF, a blood-brain penetrant, neuroactive growth factor and potent mitogen. The EGF receptor (EGFR) is expressed in the optic nerve, and preliminary data shows that EGF stimulates the proliferation of optic pathway glioma stem cells in vitro. EGFR signaling is critical for the development of other types of diet-driven tumors, including colon cancer and breast cancer, which can be driven by exposure to a high-fat (HF) diet without added sugar. Prior studies additionally show that maternal high fat (HF) diet exposure increases the proliferation of progenitors in the embryonic hypothalamus, where the Nf1-OPG cell of origin resides, similar to maternal HFHS diet exposure. HF diet and elevated EGFR signaling have also been shown to induce resistance to chemotherapeutic agents, including the Nf1-OPG therapeutic agent carboplatin. Based on these provocative findings, this application addresses the hypothesis that high dietary fat intake will increase EGF levels to accelerate gliomagenesis and induce resistance to therapy in Nf1-OPG mice. Experiments will first be performed to determine how dietary composition (fat, sugar content) affects murine Nf1-OPG formation and therapy resistance in relationship to EGF levels (Aim 1). This will be paired with mechanistic studies to determine whether EGFR signaling is required for Ob-accelerated gliomagenesis (Aim 2). Together, these experiments will determine the relationship between obesogenic diet composition, EGF and the rate of glioma formation in NF1. They will also provide a critical foundation for future investigations focused on the mechanisms by which diet affects EGF signaling to accelerate gliomagenesis in NF1.
Principal Investigators: Abby Green MD, PhD and Jeff Bednarski, MD, PhD
Description: The long-term goal of this project is to define the mutagenic processes that promote leukemic transformation of B cells in children. Precursor B cell acute lymphoblastic leukemia (ALL) is the most common hematologic malignancy in childhood. The ETV6-RUNX1 translocation is present in 25% of childhood ALL, making it the most prevalent genomic aberration among childhood leukemias. While many patients with ETV6-RUNX1-translocated ALL have favorable outcomes, the incidence of late relapse is substantial (15-20%) necessitating mechanistic understanding of disease drivers to develop improved therapeutic strategies.
The ETV6-RUNX1 translocation is an inefficient oncogene and requires additional genomic alterations to promote leukemia development. Prior studies suggest two potential sources of mutagenesis in pre-B cells with ETV6-RUNX translocations. First, RNA-sequencing of ETV6-RUNX-translocated leukemias demonstrated elevated expression of RAG endonuclease. RAG is responsible for generating purposeful DNA breaks during normal B cell development, but can cause off-target DNA damage during dysregulated states. Second, genome sequencing of ETV6-RUNX1-translocated ALLs has demonstrated an enrichment in specific mutational patterns consistent with the activity of the APOBEC3A cytosine deaminase. APOBEC3A is expressed in hematopoietic cells and restricts virus infection by mutating pathogen genomes, but when acting aberrantly can induce widespread mutations through the cellular genome. We propose that ETV6- RUNX1 translocations alter B cells in a manner that enables accumulation of mutations. We hypothesize that RAG and APOBEC3A generate genomic aberrations that drive leukemogenesis in B cells with ETV6-RUNX1 translocations. To execute the proposed studies, we have generated a novel mouse model which enables co-expression of APOBEC3A and/or RAG in hematopoietic cells with ETV6-RUNX1 translocations. The overall objective of this proposal is to determine the mechanism of leukemic transformation in B cells with ETV6-RUNX1 translocations. We hypothesize that ETV6-RUNX1 disrupts gene expression to establish an aberrant B cell state that primes cells for mutagenesis and leukemic transformation. The Aims of the project are to: 1) determine how ETV6-RUNX1 translocations alter development of pre-B cells, and 2) define how APOBEC3A promotes malignant transformation of pre-B cells.
Principal Investigator: Emily Phillips, MD
Description: Although 70% of pediatric patients with acute myeloid leukemia (AML) achieve cure, survival upon relapse is poor, with less than 50% of patients achieving a cure. Memory-like NK (ML NK) cells are NK cells upon which exposure to IL12, IL15, and IL18 induces a differentiation process in which these now ML NK cells demonstrate increased metabolic fitness and increased activation and killing of malignant cells. ML NK cells have demonstrated efficacy against pediatric AML in a phase I trial pediatric of patients with relapsed AML undergoing adoptive transfer of donor lymphocytes and ML NK cells following allogeneic stem cell transplant. Although promising, most patients do not achieve long-term survival.
The aim of the study is to improve the recognition of AML and function of ML NK cells through targeting CD33 via CD33-IL15-CD 33 trispecific killer engager (CD33 TriKE), and targeting CD123 via CD123 chimeric antigen receptor (CAR), and to determine if dual targeting of CD33 and CD123 have synergistic effect on ML NK cell responses to AML.
Design/Method: ML NK cells were co-cultured with various CD33+ and/or CD123+ AML cell lines (MOLM13, THP1, HL60, OCI-AML3). ML NK activation (degranulation, interferon gamma) was evaluated in a 6- hour functional assay. AML killing was assessed in a 4-hour flow-based killing assay. Longer-term killing potential was assessed in 20-24 hour luciferase-based assay. Transgenic IL-15 producing NSG mice were injected with THP-1 and dosed with ML NK cells, CD123 CAR-expressing ML NK cells, or ML NK cells plus CD33 TriKE every other day for 9 doses.
Preliminary Results: ML NK cells co-incubated with tumor and CD33 TriKE exhibit increased markers of activation compared to ML NK cells co-incubated with AML (MOLM13: CD107a p<.0001, IFNg p=.0056; THP1: p<.0001, IFNg p=.0015). ML NK cells treated with CD33 TriKE exhibit increased killing of AML cell lines compared to ML NK cells alone at 4 hours (absolute IC50 MOLM13 2.002 vs 4.423; THP1: 566.1 vs 2.297). There is near elimination of AML after 20 hours at E:T ratios of 10:1. In a single donor experiment, mice treated with ML NK cells plus CD33 TriKE exhibit increased tumor control and prolonged survival compared to mice receiving only ML NK cells. ML NK cells expressing CD123 CAR exhibit increased markers of activation and trend towards increased killing. Conclusion: ML NK cells targeted to CD33 via CD33 TriKE and ML NK cells targeted to CD123 via CD123 CAR exhibit increased activation and increased killing potential.
Principal Investigators: Brooke Sadler, PhD and Jorge Di Paola, MD
Description: Platelet biogenesis (a process known as thrombopoiesis) involves a sequence of complex cellular events in mature bone marrow megakaryocytes (MKs) culminating with the generation of proplatelet extensions that release platelets into the circulation. Approximately 1011 platelets must be produced daily to maintain normal concentrations of 150-400 x 109 platelets per liter of human blood. Platelets are essential not only for providing adequate hemostasis but also for being implicated in other health related processes such as inflammation, wound healing and vascular integrity.3,4 Thrombocytopenia (defined as a platelet count < 150 x 109/L) is caused by either decreased production from a variety of medical conditions such as cancer, chemotherapy and radiation therapy and aplastic anemia. Thrombocytopenia is a major clinical complication that can lead to severe hemorrhage and even death. It is estimated that more than 2 million platelet units are transfused yearly in the United States. Therefore, a better understanding of the processes that govern MK differentiation and platelet production will potentially lead to an increased ability to manipulate MKs, generate functional platelets in vitro, target therapies for congenital and chemotherapy related thrombocytopenia, and ultimately improve clinical outcomes. Our laboratory has made seminal discoveries in the genetic regulation of platelet production including the discovery of genes that cause low platelet and cancer predisposition such as NBEAL2 and ETV6. In this proposal, we will study 250 individuals from Northern India in which 15-20% of people have platelet counts of < 100 X 109/L) without significant bleeding. We will perform whole genome sequencing (WGS) and bioinformatic analyses in 250 samples, that will hopefully determine the genetic regulators that drive this thrombocytopenic phenotype and shed light on actionable targets for therapeutics.
2023 Funded Research
Principal Investigator: Hanwen Zhang, PhD
Goal: Advance a next generation theranostic pair with a novel compound, 89Zr/227Th-Lumi-PSMAUrea, for targeting imaging and alpha particle therapy of metastatic prostate cancer.
Description: Prostate cancer (PCa) is the most common non-cutaneous malignancy diagnosed in men and is their second leading cause of cancer death. Over 90 percent of these cancer cells overexpress a cell-surface protein, prostate specific membrane antigen (PSMA). Radiopharmaceuticals that target PSMA can be used to sensitively detect and characterize PCa, as well as direct cancer-specific radiation to sites throughout the body. The FDA has recently approved several PSMA-agents for imaging and targeted therapy. However, the overall survival extension of Lutetium-177 labeled therapeutics is only four months, due to the low absorbed dose at sites of disease from this low energy beta particle emitter. By developing a next generation theranostic pair with a novel compound, 89Zr/227Th-Lumi-PSMAUrea, which enables sensitive and high contrast PET imaging with 89Zr and exquisitely potent high-absorbed dose alpha particle therapy with 227Th, we seek to generate further safety and efficacy data in order to translate 89Zr-Lumi-PSMAUrea for first-in-man studies. 89Zr-Lumi-PSMAUrea PET imaging will precisely guide and predict 227Th-Lumi-PSMAUrea therapy to eradicate prostate malignancy.
Principal Investigator: Elizabeth Salerno, PhD, MPH
Goal: Determine the feasibility and preliminary efficacy of a physical therapist-delivered prehabilitation physical activity intervention to prevent cognitive decline in breast cancer patients undergoing chemotherapy, hopefully leading to a significant paradigm shift in the way we implement standard of care rehabilitation during cancer survivorship.
Description: Despite chemotherapy’s effectiveness at treating breast cancer, many patients experience severe declines in cognitive function during treatment that can persist for years. Our team’s previous research suggests that regular physical activity may help, but randomized controlled trials are necessary to confirm these findings. Our research also suggests that physical activity should begin as soon as possible after a cancer diagnosis, but most targeted physical activity interventions are designed to begin after chemotherapy completion, once cognition has already declined. Interventions delivered before or during treatment (e.g., prehabilitation) may be better suited to prevent treatment-related impairments and improve prognosis; however, these trials are difficult in practice. Oncologists have limited (if any) time to systematically advise patients on physical activity behavior, and patients are overwhelmed by a new cancer diagnosis and hesitant to begin activity on their own without proper support. Ideal models of cancer care should be pragmatic, which includes referral to physical activity programs through existing healthcare pathways to support enrollment, adherence, and long-term behavioral maintenance. To address these gaps, we propose to conduct a pilot randomized controlled trial exploring both the preliminary efficacy and feasibility of a remote, physical therapist-delivered prehabilitation physical activity intervention to prevent cognitive decline in breast cancer patients undergoing chemotherapy, compared with a wait-list control condition. Findings from this study will provide critical preliminary data for scaling our intervention to confirm the role of physical activity on cognitive function and implement pragmatic approaches to prehabilitation during treatment for breast cancer.
Principal Investigator: Jason Held, PhD
Goal: Address critical knowledge gaps in our functional and mechanistic understanding of how silencing the enzyme GSTP1 re-wires cysteine oxidation of the proteome in breast cancer, hopefully providing new ways to inhibit breast cancer growth and transformation.
Description: Glutathione S-transferase Pi 1 (GSTP1) is an enzyme that we find is uniquely and dramatically downregulated in luminal and some Her2-positive breast cancers, as well as liver and prostate cancers. This proposal will investigate how GSTP1 acts as a tumor suppressor via regulation of cysteine oxidation in proteins. This is a novel function for GTP1, so we will characterize its structure and role in cancer signaling.
Principal Investigator: Christopher Maher, PhD
Goal: Understand how our recently discovered lncRNA, RAMS11, interacts with a pioneering transcription factor to promote tumor growth and metastasis in non-small cell lung cancer patients.
Description: Lung cancer is the most common malignancy and has the highest mortality worldwide, with approximately 80-85 percent of all lung cancer patients categorized as being non-small cell lung cancer (NSCLC). Despite improvements in diagnosis and treatment options, currently only five percent of NSCLC patients with aggressive disease survive five years or longer. This represents an unmet clinical need to improve the current treatments. To address this, NSCLC research has primarily focused on understanding which genes that produce proteins, also known as protein-coding genes, have altered activity in tumor cells compared to normal cells. However, our lab recently discovered a novel class of genes that eluded researchers because, contrary to central dogma, they enable a cell to function without generating a protein (we refer to as long non-coding RNA [lncRNA] genes). Building on this discovery, our lab is focusing on how these understudied lncRNA genes enable a lung tumor to develop and eventually spread throughout the body (also known as metastases). More specifically, we recently discovered a lncRNA that becomes more active in lung cancer patients that have more aggressive disease. The current proposal will study how this lncRNA acts as a “master regulator” by interacting with specific proteins to alter their normal function and cause the original tumor to grow and spread. In the longer-term we intend to “drug” this lncRNA, ultimately leading to the development of novel therapeutics for improving outcomes in this deadly disease.
Principal Investigator: Roberto Galletto, PhD
Goal: Define the role of Pif1 in telomere maintenance in cancer cells and to identify small molecule inhibitors to test the functional outcome of Pif1 inhibition.
Description: One hallmark of cancer cells is their ability to maintain the ends of their chromosomes, in a special DNA structure called telomeres. This gives cancer cells the ability to replicate indefinitely. In general, telomere maintenance in cancer cells occurs via reactivation of a protein called telomerase, a specialized enzyme that extends the DNA length of telomeres. However, in about 10-15 percent of tumors, telomeres are maintained by a telomerase-independent pathway, termed Alternative Lengthening of Telomeres (ALT). As neither normal cells nor majority of tumors rely on ALT, specific inhibition of this pathway provides an attractive target for therapeutic intervention specifically tailored to ALT+ cancers. However, the mechanisms of ALT in human tumors and suitable targets for small molecule inhibition have remained elusive. To this end, we identify human Pif1, an enzyme that unwinds the DNA double helix and facilitates DNA replication at hard-to-replicate sites, as a candidate to be targeted for inhibition in ALT.
Principal Investigator: Ben Major, PhD
Goal: Test the pyrimenthamine drug as an inhibitor of the NRF2 protein in head and neck squamous cell carcinoma, which if proven true could result in the ability to sensitize NRF2-active cancers to standard of care chemotherapy, radiation therapy, and immune inhibition therapy.
Description: Patients suffering advanced head and neck squamous cell carcinoma (HNSCC) face poor prognoses and limited treatment options. Massive DNA sequencing efforts have revealed genes, that when mutated, contribute to HNSCC progression and resistance to chemotherapy and radiation therapy. Principle among these is the NRF2 gene, which for decades has been known to protect normal cells from stress and environmental toxins like air pollution and sun exposure. The evolution of a normal cell to a cancer cell is exceedingly stressful to cellular life, and as such, mutation and activation of NRF2 provides the growing cancer with critical survival capabilities. Moreover, HNSCC cancers with NRF2 mutations and activation have been shown to be resistant to front line chemotherapy, radiation therapy and immune-directed therapy. We recently discovered that the drug Pyrimethamine has an inhibitory effect on NRF2 activity in cell culture models and in mouse models. Mechanistically, we found that Pyrimethamine inhibits the dihydrofolate reductase (DHFR) enzyme, and that this results in inhibition of NRF2. Pyrimethamine is an FDA approved drug that has been used for decades for treatment of protozoan infections and malaria. A growing body of research shows that it has potential antitumor activity, however it has not been previously studied in HNSCC or specifically in the context of NRF2-active tumors. In this study of HNSCC patients with advanced disease, we will determine if Pyrimethamine treatment for two weeks results in loss of activity of DHFR and NRF2. If proven true, these data will support a near-future Phase 2 clinical study wherein we test whether Pyrimethamine sensitizes NRF2-active cancers to standard of care chemotherapy, radiation therapy, and immune inhibition therapy.
Principal Investigator: Aimilia Gastounioti, PhD
Goal: Our goal is to discover novel imaging phenotypes of breast cancer risk from mammography and bring effective personalized breast cancer risk models to more racially diverse screening populations.
Description: This is a study to learn whether a woman’s risk of developing breast cancer can be predicted by using computers to evaluate changes in her mammograms over time. Breast cancer risk is related to several factors, including having family members with breast cancer, certain changes in genes (mutations), and reproductive history (like number of children and breastfeeding history). Some previous studies have shown that a woman’s risk is associated with what her mammogram looks like when analyzed by a computer – looking at features of the image before a cancer is visible. However, most of these mammograms were from White women, and it is not known whether these same features can predict breast cancer risk in Black women. Because Black women are affected by more aggressive cancers that show up at younger ages, it would be particularly helpful to be able to predict breast cancer risk in this group of women. The previous studies have also looked only at features from a single mammogram. This study will look at changes in mammograms from year to year to find out whether risk can be better predicted from these changes. We will retrospectively analyze mammograms of both White and Black women in order to develop a computer program that will give a more accurate estimate of each woman’s individual risk of breast cancer, regardless of race. The ultimate goal is to improve our use of screening mammograms and lower risk of dying from breast cancer.
Principal Investigator: Ben Major, PhD
Goal: Test the pyrimenthamine drug as an inhibitor of the NRF2 protein in head and neck squamous cell carcinoma, which if proven true could result in the ability to sensitize NRF2-active cancers to standard of care chemotherapy, radiation therapy, and immune inhibition therapy.
Description: Patients suffering advanced head and neck squamous cell carcinoma (HNSCC) face poor prognoses and limited treatment options. Massive DNA sequencing efforts have revealed genes, that when mutated, contribute to HNSCC progression and resistance to chemotherapy and radiation therapy. Principle among these is the NRF2 gene, which for decades has been known to protect normal cells from stress and environmental toxins like air pollution and sun exposure. The evolution of a normal cell to a cancer cell is exceedingly stressful to cellular life, and as such, mutation and activation of NRF2 provides the growing cancer with critical survival capabilities. Moreover, HNSCC cancers with NRF2 mutations and activation have been shown to be resistant to front line chemotherapy, radiation therapy and immune-directed therapy. In this study of HNSCC patients with advanced disease, we will determine if Pyrimethamine treatment for two weeks results in loss of activity of DHFR and NRF2. If proven true, these data will support a near-future Phase 2 clinical study wherein we test whether Pyrimethamine sensitizes NRF2-active cancers to standard of care chemotherapy, radiation therapy, and immune inhibition therapy.
Principal Investigator: Ting Wang, PhD
Goal: Exploring Precision Oncology Opportunities Contributed by Transposable Elements
Description: We recently discovered that the drug Pyrimethamine has an inhibitory effect on NRF2 activity in cell culture models and in mouse models. Mechanistically, we found that Pyrimethamine inhibits the dihydrofolate reductase (DHFR) enzyme, and that this results in inhibition of NRF2. Pyrimethamine is an FDA approved drug that has been used for decades for treatment of protozoan infections and malaria. A growing body of research shows that it has potential antitumor activity, however it has not been previously studied in HNSCC or specifically in the context of NRF2-active tumors.
Principal Investigator: Hanwen Zhang, PhD
Goal: Advance a next generation theranostic pair with a novel compound, 89Zr/227Th-Lumi-PSMAUrea, for targeting imaging and alpha particle therapy of metastatic prostate cancer.
Description: Prostate cancer (PCa) is the most common non-cutaneous malignancy diagnosed in men and is their second leading cause of cancer death. Over 90 percent of these cancer cells overexpress a cell-surface protein, prostate specific membrane antigen (PSMA). Radiopharmaceuticals that target PSMA can be used to sensitively detect and characterize PCa, as well as direct cancer-specific radiation to sites throughout the body. The FDA has recently approved several PSMA-agents for imaging and targeted therapy. However, the overall survival extension of Lutetium-177 labeled therapeutics is only four months, due to the low absorbed dose at sites of disease from this low energy beta particle emitter. By developing a next generation theranostic pair with a novel compound, 89Zr/227Th-Lumi-PSMAUrea, which enables sensitive and high contrast PET imaging with 89Zr and exquisitely potent high-absorbed dose alpha particle therapy with 227Th, we seek to generate further safety and efficacy data in order to translate 89Zr-Lumi-PSMAUrea for first-in-man studies. 89Zr-Lumi-PSMAUrea PET imaging will precisely guide and predict 227Th-Lumi-PSMAUrea therapy to eradicate prostate malignancy.
Principal Investigator: Armin Ghobadi, MD
Goal: Our goal is to determine if adding the targeted oral drug duvelisib to standard treatment with genetically modified immune cells (chimeric antigen receptor or “CAR” T cells) will decrease cellular immunotherapy-related side effects and help CAR T cells to more effectively kill non-Hodgkin lymphoma.
Description: Non-Hodgkin lymphoma is the most common blood cancer in adults. It develops from the lymphatic glands, which form an important part of the immune system. Currently, the first treatment patients receive for this cancer is high doses of chemotherapy, which can cure about half of patients. However, if the lymphoma does not disappear after chemotherapy or comes back after treatment, additional chemotherapy treatments are unlikely to provide a cure. Physicians are increasingly interested in harnessing the body’s own immune system to help fight cancer, including lymphoma. One promising approach is the collection and modification of the patient’s own immune cells to make a special type of anti-cancer treatment called chimeric antigen receptor T cells or “CAR T cells”. These cells are specifically designed to find and destroy lymphoma cells after recognizing a specific protein on their surface. In prior studies, the use of CAR T cells has been shown to cure about a third of patients with NHL who were not cured by chemotherapy. Unfortunately, this therapy can have significant side effects that require hospitalization or admission to the intensive care unit, including fevers, confusion, difficulty breathing and low blood pressure. Further, the majority of patients are still not cured by this approach and most treatments are ineffective if the lymphoma comes back after receiving CAR T cell therapy. Consequently, our study proposes to use duvelisib, a medicine that can be taken by mouth, to improve the function of CAR T cells during treatment. Based on work in the laboratory, we believe it will decrease the side effects of CAR T cell treatment while helping CAR T cells to last longer and kill cancer cells better. With this approach, we hope to increase the number of patients who can safely receive CAR T cells and provide better control of the cancer, ultimately leading to more patients with lymphoma being cured.
Principal Investigator: Kian-Huat Lim, MD, PhD
Goal: Our goal is to improve the efficacy of treatment for patients with metastatic gastric and esophageal cancers by combining a new drug called CA-4948 with current chemo-immunotherapy treatments to activate killer T cells.
Description: Chronic inflammation is an important risk factor that leads to the development of gastrointestinal cancers including gastric, esophageal, pancreatic, and colon cancers. Under the microscope, we can easily observe that these cancers are heavily surrounded by inflammatory cells. These inflammatory cells secrete soluble factors that not only fuel cancer cell growth, but also block our bodies’ main immune defense mechanism, particularly the killer T cells. We have recently identified IRAK4, an enzyme within cancer cells, as a key target that drives chronic inflammation in gastrointestinal cancers. We found that blocking IRAK4 using a new drug called CA-4948 can dramatically decrease inflammatory cells inside the cancer of experimental mouse models, causing the killer T cells to be partly activated. When we added an immunotherapy agent called anti-PD1 antibody, we observed a further boost in killer T cell activity and number, which led to complete elimination of cancers in more than half of the experimental mice. This is an exciting finding that led us to open a new clinical trial for patients with metastatic gastric and esophageal cancers, in which chemotherapy and immunotherapy are already part of the regimen. Our hope is that adding CA-4948 will make these therapies more effective and last longer in patients. To our best knowledge, this is the first clinical trial that combines CA-4948 with chemo-immunotherapy in cancer patients. If shown to be effective from this study, we will proceed to open this clinical trial in a larger scale in collaboration with other cancer centers in the future.
Principal Investigator: Roberto Galletto, PhD
Goal: Define the role of Pif1 in telomere maintenance in cancer cells and to identify small molecule inhibitors to test the functional outcome of Pif1 inhibition.
Description: One hallmark of cancer cells is their ability to maintain the ends of their chromosomes, in a special DNA structure called telomeres. This gives cancer cells the ability to replicate indefinitely. In general, telomere maintenance in cancer cells occurs via reactivation of a protein called telomerase, a specialized enzyme that extends the DNA length of telomeres. However, in about 10-15 percent of tumors, telomeres are maintained by a telomerase-independent pathway, termed Alternative Lengthening of Telomeres (ALT).
Principal Investigator: Elizabeth Salerno, PhD, MPH
Goal: Determine the feasibility and preliminary efficacy of a physical therapist-delivered prehabilitation physical activity intervention to prevent cognitive decline in breast cancer patients undergoing chemotherapy, hopefully leading to a significant paradigm shift in the way we implement standard of care rehabilitation during cancer survivorship.
Description: Despite chemotherapy’s effectiveness at treating breast cancer, many patients experience severe declines in cognitive function during treatment that can persist for years. Our team’s previous research suggests that regular physical activity may help, but randomized controlled trials are necessary to confirm these findings. Our research also suggests that physical activity should begin as soon as possible after a cancer diagnosis, but most targeted physical activity interventions are designed to begin after chemotherapy completion, once cognition has already declined. Interventions delivered before or during treatment (e.g., prehabilitation) may be better suited to prevent treatment-related impairments and improve prognosis; however, these trials are difficult in practice. Oncologists have limited (if any) time to systematically advise patients on physical activity behavior, and patients are overwhelmed by a new cancer diagnosis and hesitant to begin activity on their own without proper support. Ideal models of cancer care should be pragmatic, which includes referral to physical activity programs through existing healthcare pathways to support enrollment, adherence, and long-term behavioral maintenance. To address these gaps, we propose to conduct a pilot randomized controlled trial exploring both the preliminary efficacy and feasibility of a remote, physical therapist-delivered prehabilitation physical activity intervention to prevent cognitive decline in breast cancer patients undergoing chemotherapy, compared with a wait-list control condition. Findings from this study will provide critical preliminary data for scaling our intervention to confirm the role of physical activity on cognitive function and implement pragmatic approaches to prehabilitation during treatment for breast cancer.
Principal Investigator: Sheila Stewart, PhD
Goal: Our goal is to develop smarter breast cancer therapies that have a more potent effect at limiting disease progression by interrogating how age-related changes in non-tumor cells contribute to increases in breast cancer.
Description: As neither normal cells nor majority of tumors rely on ALT, specific inhibition of this pathway provides an attractive target for therapeutic intervention specifically tailored to ALT+ cancers. However, the mechanisms of ALT in human tumors and suitable targets for small molecule inhibition have remained elusive. To this end, we identify human Pif1, an enzyme that unwinds the DNA double helix and facilitates DNA replication at hard-to-replicate sites, as a candidate to be targeted for inhibition in ALT.
Principal Investigator: Patricia Ribeiro Pereira, PhD
Goal: Our goal is to enhance the efficacy of immunotherapy treatments in gastric tumors. We aim to use molecular imaging techniques to investigate the mechanisms of cancer-cell surface protein regulation to enhance immune checkpoint blockade efficacy in gastric tumors.
Description: Cancer cells can become invisible to monoclonal antibody drugs (i.e., a form of immunotherapy) by decreasing the availability of cancer-cell surface proteins, which are the ones targeted by these drugs. We have recently shown that proteins present in high quantities in gastric cancer cells are not always available at the cell surface for the effective binding of antibody drugs. The processes by which proteins are distributed throughout the cancer cell and internalized from the cell membrane could explain why immunotherapies only work in 30% of patients with gastric cancer. Thus, there is a critical need to understand the biological mechanisms of cancer-cell surface protein regulation and develop approaches that allow effective control of these processes. The Disease Imaging and Therapy lab uses cutting-edge imaging technologies to visualize in the whole body and in real-time the biological processes by which proteins are internalized into the gastric cancer cell and away from the membrane where antibody drugs bind to them. We then develop pharmacologic approaches to control these processes in ways that enable the conversion of non-responder gastric cancers into responders. This proposal aims to use our imaging methodologies to discover the membrane trafficking mechanisms of PD-L1—an important membrane protein that prevents immune cells from destroying cancer cells—and determine whether PD-L1 trafficking can be modulated to enhance the efficacy of antibody drugs targeting PD-L1 in gastric cancers. These approaches will enhance antibody therapies targeting cell-surface receptors and increase the number of patients that benefit from them.
Principal Investigator: Chris Maher, PhD
Goal: Understand how our recently discovered lncRNA, RAMS11, interacts with a pioneering transcription factor to promote tumor growth and metastasis in non-small cell lung cancer patients.
Description: Lung cancer is the most common malignancy and has the highest mortality worldwide, with approximately 80-85 percent of all lung cancer patients categorized as being non-small cell lung cancer (NSCLC). Despite improvements in diagnosis and treatment options, currently only five percent of NSCLC patients with aggressive disease survive five years or longer. This represents an unmet clinical need to improve the current treatments. To address this, NSCLC research has primarily focused on understanding which genes that produce proteins, also known as protein-coding genes, have altered activity in tumor cells compared to normal cells. However, our lab recently discovered a novel class of genes that eluded researchers because, contrary to central dogma, they enable a cell to function without generating a protein (we refer to as long non-coding RNA [lncRNA] genes). Building on this discovery, our lab is focusing on how these understudied lncRNA genes enable a lung tumor to develop and eventually spread throughout the body (also known as metastases). More specifically, we recently discovered a lncRNA that becomes more active in lung cancer patients that have more aggressive disease. The current proposal will study how this lncRNA acts as a “master regulator” by interacting with specific proteins to alter their normal function and cause the original tumor to grow and spread. In the longer-term we intend to “drug” this lncRNA, ultimately leading to the development of novel therapeutics for improving outcomes in this deadly disease.
Principal Investigator: Melissa Mavers, MD, PhD
Goal: The goal is to improve existing cellular therapies as well as develop novel cellular therapies for malignant diseases by supporting the development of novel invariant natural killer T (iNKT) cell-based cancer-targeting therapies with enhanced safety and efficacy.
Principal Investigator: Bryan Sisk, MD, MSCI
Co-Investigator: Albert Lai, PhD
Goal: The goal is to develop cancer-specific and vascular anomaly-specific chatbots using a retrieval-augmented generation approach and assess the usefulness, quality and acceptability of these tools.
Principal Investigator: Jorge Di Paola, MD
Goal: The goal is to understand the biological significance of these genetic defects, and their potential impact on human disease.
Principal Investigator: Margaret Ferris, MD, PhD
Goal: The goal is to further understand the molecular mechanism of the retinoid receptor/COMPASS-like complex interaction as well as to develop pre-clinical data for a clinical trial of combination menin inhibitor and retinoids.